Testicular cancer awareness month is recognized in April. So this post is to help raise awareness of testicular cancer.
This isn’t talked about as much as other cancers. It seems like talking about it is taboo.
But it’s important to educate those at risk and remove the stigma.
It can affect anyone who has testicles, including men, transgender (trans) women, and people assigned male at birth.
Testicular cancer can be found through monthly self-examinations.
We see a lot of promoting breast self-exams but not so much about testicular exams.
When it’s caught in an early stage, this cancer is easily treatable.
Understanding the Testes
Testicular cancer occurs in the testicles (testes).
These oval-shaped organs are located inside the scrotum, a loose bag of skin underneath the penis.
The testicles produce testosterone and sperm for reproduction.
Types of Testicular Cancer
Almost all testicular cancers start in germ cells in the testicles. Germ cells are the ones that produce sperm.
The two main types of testicular germ cell tumors are seminomas and non-seminomas.
Non-seminomas are made up of different types of cells. They tend to grow and spread more quickly than seminomas.
Another rare type of testicular cancer is a type of non-Hodgkin lymphoma.
Statistics/Fast Facts
Testicular cancer is the most common cancer in 20-35-year-old men.
According to the American Cancer Society, approximately 9,760 new cases will be diagnosed this year in the United States.
Around 460 die in the U.S. each year from the disease.
The National Cancer Institute (NCI) states the five-year survival rate for testicular cancer is about 95 percent.
That makes it one of the most treatable types of cancer.
The incidence rate of testicular cancer has been rising in the US and other countries for decades. The reasons for this are unknown.
Risk Factors
Many young men and middle-aged men who develop testicular cancer have no risk factors at all.
Some known risk factors include:
- abnormal testicular development, including an undescended testicle.
- a family history of testicular cancer, especially if it’s a father or brother
- White men are at higher risk than other ethnicities
- congenital (means you’re born with it) abnormalities with the penis or kidneys
- Human Immunodeficiency Virus (HIV) infection
Symptoms of Testicular Cancer
The most common symptom of testicular cancer is a painless lump or swelling in a testicle.
Other symptoms can include:
- discomfort or pain in the scrotum
- a dull ache in the groin, lower abdomen, or back
- a sudden buildup of fluid in the scrotum
- breast swelling or tenderness in the nipples or breasts
Diagnosis
There are no official screening tests for testicular cancer. Monthly testicular self-exams should be done so you know what’s normal and not normal with your testicles.
Compare one testicle with the other. Look for any changes from the last monthly exam.
Your healthcare provider should also perform a testicular exam at your annual physical.
The Testicular Cancer Awareness Foundation has created this great graphic to follow for monthly self-exams.
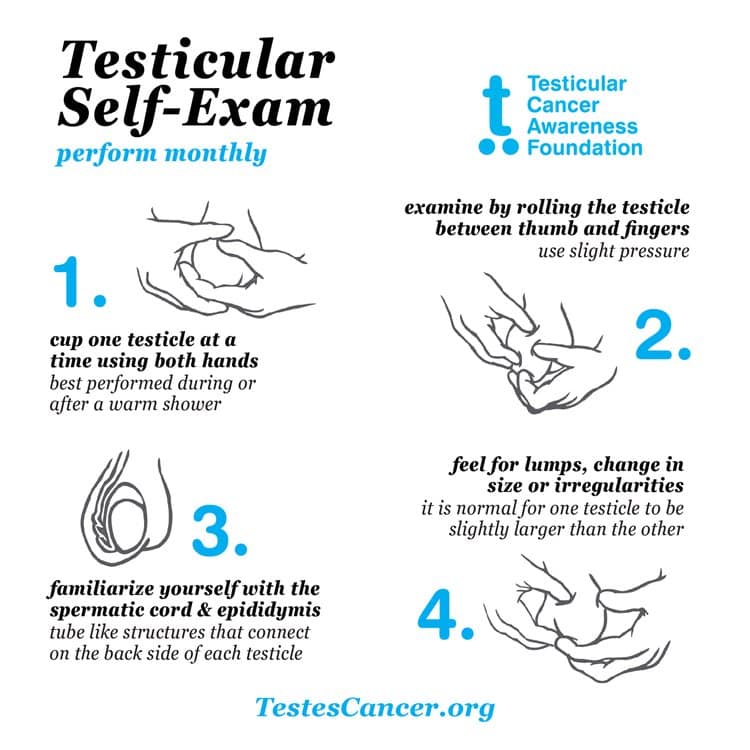
If you feel like something is wrong, your health care provider will perform an exam.
They’ll likely arrange for blood tests and an ultrasound.
If something is found, the only way to get a diagnosis is to have surgery.
The affected testicle will likely need to be removed.
A doctor, called a pathologist, will examine the testicle tissue and look for cancer cells.
You may also have blood tests done to check tumor marker levels.
Treatment of Testicular Cancer
The 3 main treatments for testicular cancer are:
- surgery
- chemotherapy
- radiation therapy
The type and amount of treatment options will vary depending on;
- whether it’s a seminoma or non-seminoma
- if the cancer has spread outside the testicle
- if you are at high risk of testicular cancer returning
Note that if testicular cancer comes back, it can usually be treated successfully.
Removing the testicle removes the cancer.
The surgery won’t affect the ability to get an erection or fertility, which is the ability to have children in the future.
Conclusion
Self-examination of the testes is the most common method of early detection. This also gives the highest chance of the cancer being treated successfully.
If you notice something off, especially if you have a family history of the disease, call your doctor so further tests can be run.
If you are diagnosed with testicular cancer, the good news is that this is easily treated.
If caught early, surgery removes the cancer, and that may be all the treatment you’ll need.
If you’re dealing with testicular cancer or are a caregiver to someone with testicular cancer and need extra support, let me know.
I’d be happy to help and walk with you through this journey.